Coronary Angioplasty
Coronary Angioplasty, also known as Percutaneous Coronary Intervention (PCI), is a minimally invasive procedure used to open up blocked or narrowed coronary arteries, restoring normal blood flow to the heart muscle. It is commonly performed to treat coronary artery disease (CAD), which can cause chest pain (angina), shortness of breath, and increase the risk of heart attacks. Angioplasty is often performed as an emergency treatment during a heart attack or as a planned procedure after diagnostic tests like coronary angiography.
Steps Involved in Coronary Angioplasty
- Preparation:
- Before the procedure, the patient undergoes initial evaluations, including blood tests, electrocardiograms (ECG), and sometimes echocardiograms.
- The patient is awake but sedated, and a local anesthetic is applied at the catheter insertion site, usually in the groin (femoral artery) or wrist (radial artery).
- Catheter Insertion:
- A small incision is made, and a sheath is inserted into the artery.
- A thin, flexible tube called a guide catheter is threaded through the sheath into the artery and guided toward the coronary arteries.
- Real-time X-ray imaging (fluoroscopy) is used to monitor the catheter’s movement through the vascular system.
- Guidewire Placement:
- A soft, flexible wire called a guidewire is inserted through the catheter and advanced into the blocked coronary artery.
- The guidewire helps position the balloon catheter at the site of the blockage.
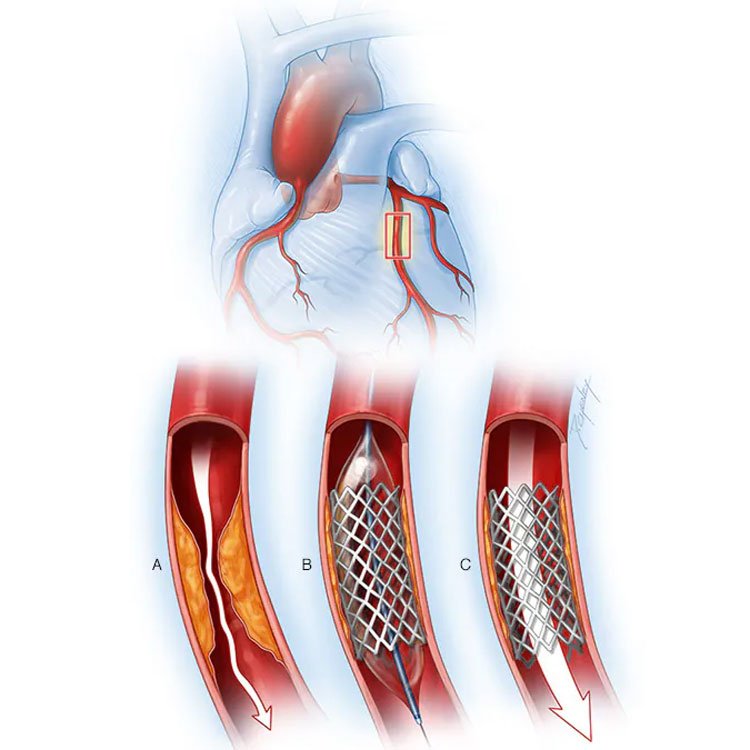
- Balloon Inflation:
- A second catheter, equipped with a small balloon at its tip, is advanced over the guidewire to the blockage.
- Once in place, the balloon is inflated, compressing the fatty plaque or blockage against the artery walls. This widens the artery, allowing blood to flow more freely.
- Stent Placement (Optional but Common):
- In many cases, a stent (a small, wire mesh tube) is placed at the site of the blockage. The stent is mounted on the balloon catheter, and when the balloon is inflated, the stent expands and is embedded in the artery wall.
- Stents are often drug-eluting stents (DES), coated with medication to prevent scar tissue from forming and re-blocking the artery. Some are bare-metal stents (BMS), which do not have medication.
- Balloon Deflation and Catheter Removal:
- After the balloon is deflated and the stent is secured in place (if used), the catheter and guidewire are removed.
- Blood flow is immediately restored in the treated artery, and the sheath is removed from the insertion site.
After the Procedure
- The patient is monitored in a recovery area to ensure that there are no complications, such as bleeding at the catheter insertion site or an allergic reaction to the contrast dye.
- Most patients stay in the hospital for 12-24 hours, depending on their overall condition, but some may be discharged the same day.
- Blood-thinning medications (antiplatelets) are prescribed to prevent blood clots from forming in the stent.
Recovery and Lifestyle Changes
- Full recovery from angioplasty usually takes about a week, with recommendations to avoid strenuous activity during that time.
- Long-term lifestyle changes, such as a heart-healthy diet, regular exercise, quitting smoking, and managing stress, are vital for preventing future artery blockages.
- Medications to control cholesterol (statins), blood pressure, and other conditions are often prescribed after the procedure.
Risks and Complications
Though coronary angioplasty is a common and generally safe procedure, there are some risks involved:
- Bleeding or infection at the catheter insertion site which are very rare.
- Restenosis: Narrowing of the artery again, especially in cases where a stent is not used.(rare)
- Blood clots: Rarely, blood clots may form in the stent.(rare)
- Heart attack or stroke during or shortly after the procedure (rare).
- Artery damage: In very rare cases, the artery may be injured during the procedure, necessitating emergency surgery.(very very rare)
Benefits
Coronary angioplasty has several key benefits:
- Immediate relief from chest pain (angina).
- Reduced risk of heart attack.
- Improved blood flow to the heart muscle, leading to better heart function.
- Faster recovery time compared to open-heart surgery (such as coronary artery bypass grafting, or CABG).
Conclusion
Coronary angioplasty is a life-saving procedure for patients with blocked coronary arteries, offering relief from symptoms, improved quality of life, and reduced risk of heart attacks. With advancements in stent technology and imaging techniques, angioplasty has become a common and effective treatment for coronary artery disease.
Youtube link – https://www.youtube.com/watch?v=MKRGgX5rYbY
